By Fiscal Year (FY) 2024, financial projections show the District will deplete its reserves and begin to operate at a deficit unless an alternate revenue source is identified or the District reduces the level of service and protection it currently provides; this includes cutting emergency medical service (EMS), transport services, and accepting increased response times to emergencies in the community, including the city of Pflugerville. This is the result of a disproportionate growth in service demand and lack of adequate funding for EMS. Additional revenue growth limitations put in place by the legislature have compounded the problem. District staff has identified an estimated $6 million dollar shortfall in FY2024, which would be required to maintain current service levels.
The District is legally permitted, but not required by law, to provide EMS. The District began working towards a solution for EMS in the community in 2010. In 2010, staff began seeing increased Austin Travis County EMS ambulance response times. At that time, the District was providing basic life support (BLS) first response in the community. BLS care is where firefighters, who are all emergency medical technicians (EMTs), provide basic life saving measures such as airway procedures, non-pharmacological cardiopulmonary resuscitation, non-invasive medical treatment, and limited trauma care. First response refers to the initial response to a medical emergency that typically arrives well in advance of ambulances with transport capability. BLS service is delivered via firefighters arriving on a fire apparatus. BLS is a critical component of the EMS system, along with advanced life support (ALS), and transport service as the other two components. ALS is typically delivered by a paramedic and includes physician level airway procedures, broad range pharmacology administration that can quickly improve life threatening conditions, and includes advanced clinical decision making made in the field to determine the patient’s condition and needs. ALS is usually delivered by a paramedic on an ambulance, but can also be delivered by firefighters many of which are also trained as paramedics.
Staff has identified four options as potential solutions for the financial problem facing the District. The District has already implemented traditional government budget reduction procedures to include: evaluation of all operational programs and services which reduced the operations budget by 12% in FY2021. Service and user fees were also evaluated and updated for FY2021. These changes will positively impact the budget by reducing spending and increasing revenue. However, these two significant, and unpopular, changes will not solve the projected budget deficit.
District leadership is trying to solve a very complex problem with regard to adequately funding EMS and is at a point where the community and local stakeholders must be engaged in working together towards a solution for the benefit of the community as a whole. The District is prepared to implement all of these options, but our hope is that a community-based solution that is both logical and beneficial is reached.
In May 2020 Board President Mike Bessner appointed Commissioners April Griffin and Mike Howe to work with staff in a subcommittee to identify options to handle the upcoming financial problem for the District, and how to best address adequately funding EMS in the community. The collective work of this committee produced four potential options. These options were presented to the board in July 2020.
The four options are:
Option 1 – Do nothing. This option does not solve the problem. Response times will continue to grow and will lead to negative emergency outcomes, increased maintenance costs, additional workload on firefighter/paramedics, recruitment and retention problems. It will eventually lead to Option 2.
Option 2 – Reduce or eliminate services. The District ceases providing EMS. The City of Pflugerville and/or Travis County would need to provide these services at their own cost.
Option 3 – Establishment of an agreement between the District, the City of Pflugerville, and Travis County to provide at least $6 million in supplemental funding annually to sufficiently maintain current levels of advanced life support and EMS transport service provided by the District.
Option 4 – Voter driven creation of an overlay district to fund EMS and preserve advanced life support and EMS transport service the community currently receives.
For-profit ambulances or private EMS are another option that was investigated. This option comes with significant changes in performance and the quality of service provided. In the District’s professional analysis, this is the worst choice for the community for 911 services, but recognized as the appropriate service provided for non-emergency related needs.
Each option was thoroughly investigated in order to examine the impacts of each to the organization and community. District staff are fully prepared to implement each option, or a combination of options.
Austin/Travis County EMS (ATCEMS) previously provided inadequate service to the area. They were only able to provide two ambulances. The second ambulance came only after requests from ESD2 for more units to meet response time goals, and ultimately the second ambulance still did not meet the demand. Both of these ambulances were unavailable 44% of the time while they were either on medical calls in the District or the City of Austin.
An outside consultant, the Medical Advisory Group (MAG), examined the problem with Austin/Travis County EMS providing service to Travis County. Some of the findings and recommendations from the “Pre-Hospital Emergency Medical Care Study” were that ATCEMS was not meeting response times in the county (ESD2), county taxpayers had no control in labor costs for City of Austin labor, and that fire based EMS transport service delivered by ESDs are a cost effective option to be explored.
Three other ESDs in Travis county have EMS overlays and have experienced success in addressing adequate funding for EMS. We also want to be clear that we believe the men and women of Austin/Travis County EMS are incredible medical providers and acknowledge that they also face a challenge trying to keep up with growth in the City of Austin and many portions of Travis County. To this day we maintain a great working relationship with ATCEMS. They dispatch our ambulances and serve as our back up when all of our units are out on calls. We appreciate and value these services.
No. The financial forecast shows construction of Station 6 and 7 and related staff equipment being the largest increased expense to our future financial situation – most of that cost is for staffing and apparatus. The reason we still have a financial issue even with potential to add 2 ATCEMS units is because the District is already shouldering the cost for 5 ambulances to meet the current demand and adding 2 ambulances will not provide any financial relief for those costs already shouldered and invested in by the District. This funding could be used to focus solely on the fire/rescue mission only, but instead is being used to provide EMS transport service in the District. Keep in mind ATCEMS still struggles to meet response times in other less populated parts of Travis County along with the growing call demand in the city of Austin.
The funding that ESD2 taxpayers pay to Travis County that is then paid to ATCEMS should be returned to ESD2 since the District is providing EMS transport services. The District has requested this with no success. This would help with the District’s financial problem with regard to EMS transport services. This allows for local input by taxpayers for EMS transport services. Additionally, the District has a deployment standard that meets response time goals and has a more efficient cost per ambulance- by taking advantage of cost saving by using firefighter/EMTs and paramedics who are already located and working in the community.
We are in the process of doing this very unpopular practice. However, even significant increases in fees will not fund EMS adequately. Those covered by Medicare are limited as Medicare has a limit that it will pay for EMS transport. Keep in mind many of the citizens we serve are below the poverty line and are unable to pay.
4. Won’t commercial growth cover the expenses?
Certainly commercial growth helps, but let’s take a large commercial center for example – Let’s assume it goes on the tax rolls at $250 million in property value. At the maximum ESD tax rate of 10 cents per $100 of assessed value, that will generate $250,000 in tax revenue annually for the ESD. That won’t quite cover half of the cost of what it takes to operate a single ambulance. Keep in mind the 1,000 plus people employed and the increased traffic it will generate (vehicle accidents), which increases the number of incidents the District must respond to. Those 1,000 people will also need places to live- resulting in more residential service demand.
5. Is an EMS overlay district a separate tax?
Yes, an overlay would create a separate taxing entity to fund EMS. For a home on the tax rolls at $257,000, the additional tax would be about $154/year or about $13 a month.
6. What would the boundaries of an EMS overlay district be?
Same as current ESD 2 boundaries.
7. What would the tax rate for an EMS overlay district be?
The petition would request what the Texas Constitution allows; a max of 10 cents per $100 of assessed property value. However, based on conservative pro forma analysis we believe it may be between 6-7 cents per $100 of property value. The actual rate would be decided by the new district’s Board of Commissioners.
8. If a new EMS overlay district is created, would taxes go down in ESD 2?
No, the current funding for ESD2 provides fire and rescue services. Due to the ever increasing number of incidents, these costs are not going down. The current funding model is appropriate to fund these services only, not the additional EMS transport services. This funding must be continued in order to provide fire and rescue services to the growing community.
9. What would the incremental costs of an EMS overlay district be?
We have projected a 3% per year revenue growth in FY24 and FY25 to project potential property value increases and keep below the 3.5% revenue growth established by Senate Bill 2. If growth and value trends continue, this additional revenue will come as a result of property value increases or additions of new property. Assuming the tax rate was set at $0.04 per $100 and if values don’t increase and there are no new properties then we would propose a tax rate increase. To increase the revenue in FY24 by 3% the tax rate would be approximately $0.0412 and FY25 $0.0424.
Yes, a pro forma can be seen here.
No matter how you divide it, the current revenue streams, even when combined for obvious economies of scale, cannot meet the demand. Splitting the ESD would actually further limit and reduce services by reducing funding available to pay for these services through resource pooling. Smaller ESDs struggle to provide basic fire/rescue services at all, let alone additional expensive services such as EMS transport services. Third party analysis by consultants, such as the MAG report, actually recommend doing the opposite, whereas consolidation provides economies of scale by combining ESDs. This would also be a significant legal undertaking and would be costly in terms of legal expenses.
Current projections show that revenues equal to an additional 6.5 cents per $100 assessed property value would be adequate to maintain our current level of enhanced emergency medical care and ambulance service for the foreseeable future. For a home on the tax rolls at $257,000, the additional tax would be $154/year or about $13 a month.
In accordance with state law, ESD2 is overseen by a volunteer citizen board of five commissioners. All of them are residents and taxpayers of the District and are appointed by the Travis County Commissioners Court and serve two year terms. All ESD commissioners in Texas are required to take six hours of training in District operations that is accredited by an institution of higher learning every two years.
The advantages of options 2 and 3 are that, even though residents’ access to advanced life support or ambulance might be diminished, there would be no additional direct ESD taxation to pay for those services; other government entities would have to step up and pay through their own funding sources. It will be difficult to get other government funding to pay for EMS and ambulance transport. Like ESD2, other government agencies are facing financial difficulties to provide their own services dealing with the effects of Senate Bill 2. They also are facing limits on increasing their revenues and might prevent them from providing support. On option 4 under state law, Commissioners on one ESD may be appointed to serve on the board of an overlay ESD. The disadvantage of option 4 is if the Travis County Commissioner’s Court chose not to appoint the same board members to both ESDs, coordination could suffer and conflicts between the two boards could occur.
First, and foremost, ESD2 is a separate governmental entity from the City of Pflugerville. We exist solely for fire/rescue services. We do not provide police, parks, water, or roads. While our fire engines and ambulances drive on those roads too, and we’d like them improved, we aren’t responsible for building or maintaining them. In terms of fire and EMS protection to the east side of Pflugerville we have a sixth fire station in the construction phase located on Weiss Lane by Weiss High School. We also have identified sites in the Hodde Lane and Cameron Road areas to plan for station 7. The two stations will bring much needed resources to the eastern part of Pflugerville. Additionally, we look forward to automatic aid agreements with the City of Round Rock and Hutto to assist as well.
The creation of an EMS overlay district to assure adequate funding for advanced life support and ambulance transport would not necessarily create any new jobs. As currently envisioned, the new ESD – Travis County Emergency Services District No. 17 – would contract with the existing ESD to provide services. While jobs wouldn’t necessarily be created, they could be preserved, and jobs could be added in the future for growth. Without additional funding, ESD 2 would have to cut services to continue to be financially viable. Since most of the ESD 2 budget is personnel costs, cutting the budget means cutting positions.
While our firefighters and paramedics are dealing with everything the general public is also dealing with regarding: homeschooling, childcare, and the associated stresses – their commitment to serving the public has not wavered from the start of the pandemic. Not once. District staff have remained committed to their oaths to serve the public and meet the challenge head on. They have responded to over 500 COVID-19 related calls to date and are able to skillfully and safely navigate the additional challenges of working in a pandemic as frontline healthcare providers. The Commissioners and Fire Chiefs are incredibly proud of their faithful service, and noted their courage early in the pandemic. District leadership has several meetings with the firefighters, including the Association President at least weekly, to ensure staff are taken care of and are doing ok. Our staff’s safety and ability to deliver high levels of service remain our top priority because we care.
COVID-19 has impacted nearly every part of our operation. From new procedures on how to prepare, respond, and treat COVID-19 patients, to increased decontamination procedures, and additional expenses for PPE, supplies, and overtime. We have had to make adjustments to all of our incident responses. We are monitoring our sick call more stringently, have had to redirect some staff to assist with this, and have had a few firefighters contract the virus off duty (all experiencing relatively minor effects, and all are back at work). We have nearly all of our civilian staff working remotely with very few exceptions, and we had to place some employees on furlough do the inability to continue their work in the current challenging environment. To this day, the District continues to respond to COVID related calls, and is operating in a declared disaster state utilizing an incident command system each day for planning, responding, and documentation as required by that system. For smaller scale incidents this can require a dedicated staff of at least 5 staff positions generating numerous pages of required documentation. District staff is having to do this daily with existing staff on top of normal job duties. We continue to monitor the situation daily by attending multiple meetings and information sessions with all of our local, state, and national partners.
The simple answer is an increased time in our ability to get to your emergency in a timely manner, which would negatively impact our ability to successfully resolve your emergency. For example, in a cardiac arrest scenario, which the District responds to about 160 of these incidents each year, or about 1 every other day. Research done by W. Ibram that was published in the National Center for Biotechnology Information explained that with every minute without CPR, survival from cardiac arrest decreases by as much as 10%. Additionally, research published in the Annals of Emergency Medicine and the Journal of the American Medical Association by M.P. Larsen, et al. titled, “Predicting Survival from Out of Hospital Cardiac Arrest: A Graphic Model”, showed that:
We want to have the best possible chance to positively affect incident outcomes and getting to an emergency in a timely manner is critical to doing that.
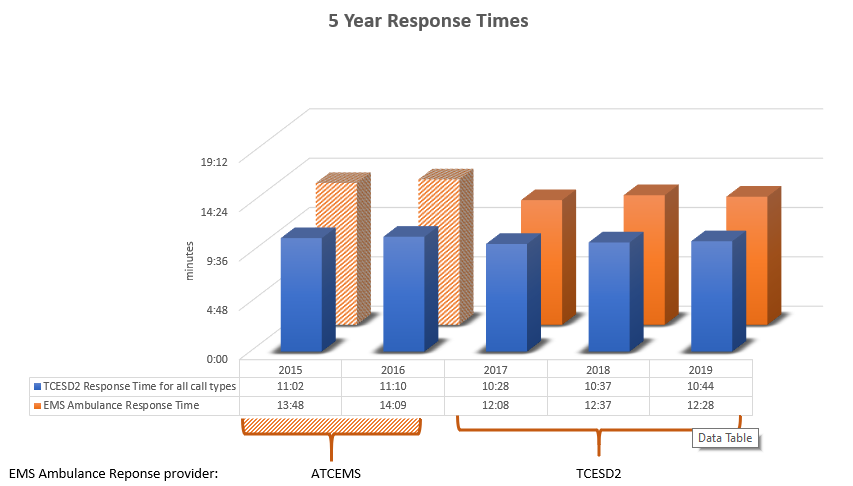
Here is a summary of the districts aggregate response times over the past five years:
The simple answer is there is a negative effect on staff because of the increased call volume. Additional time spent on emergency calls, without an increase in resources, places additional workload on existing staff. This reduces the amount of time that is needed for other required activities such as risk reduction, public education, preventative maintenance, and mandated training. This can also lead to safety issues related to accidents and decision making by overworked staff.
We have always traditionally been a busy fire department based on the lean operational management philosophy of District leadership. Most of our tenured firefighters and officers grew up fighting fires with limited resources. We called it going John Wayne. We have certainly evolved and look at this a lot differently today based on the size and complexity of our community, advances in safety and technology, and what we know about health and safety of firefighters; including the long term consequences of overworking staff.
Working on an ambulance is one of the most challenging aspects of this job. Firefighter EMTs and paramedics working on ambulances typically work longer periods on emergency incidents because of the number of medical calls vs the available ambulances, and then the added time it takes to transport, and drop a patient off at the hospital, complete required documentation, and then get the ambulance back in service. So in an optimal situation we would rotate our staff on a regular basis to help alleviate the workload. However, we have to have the right number of highly trained and qualified personnel in order to do this.
This is challenging to do for several reasons. The first being our original plan was to be implemented over four years beginning in 2017. We had planned to introduce an ambulance per year for four years. Once the City of Austin made the decision to relocate their ambulances, we had to fast track that plan. We had the minimal staffing, but didn’t have the optimal staffing to do this, but as usual our folks stepped up. They continue to do this to this day. We have slowly been able to increase our staffing to improve this, but hiring, training, and keeping qualified paramedics is a challenge. We monitor our utilization, or workload balance, very closely. While we maintain lower utilization than a third party service or for-profit system, taking into account everything we must do, our folks are busy.
We are confident that if we receive the adequate funding we can get to an optimal staffing level. However, if we can not solve this problem, the workload will need to be addressed for several reasons related to the safety of staff and the ability to treat patients effectively. Our people are amazing and among the best in the business, but they are not invincible, and they are not robots.
For Additional Information
https://www.youtube.com/watch?v=i1X0eFz0KKc&t=26s
https://drive.google.com/file/d/17iPNBGB7I2_VedqZjPWjziZ36vp1ZVvZ/view?usp=sharing
https://drive.google.com/file/d/1wBJD_bkepegPTCTKHW1JX1ofh0w8AI2e/view?usp=drivesdk
4. Townhall power point presentation
https://docs.google.com/presentation/d/1tP-yILqOTp_l5hhiyC0c4RrCawXt1cHC6q1bTbN-5ik/edit?usp=sharing